Para saber más sobre degeneración macular y enfermedades de la retina:
Age-Related Macular Degeneration and
Retinal Diseases
You can add subtitles or change the language by clicking on the “cc” button on the video.
What is AMD?
Age-related macular degeneration (AMD) is a progressive disease that affects the macula, the central part of the retina responsible for sharp, detailed vision. This area is essential for daily activities such as reading, recognizing faces, driving, or distinguishing colors clearly. AMD is one of the leading causes of vision loss in people over 55 worldwide.
What are the symptoms?
Common symptoms include:
- Blurry or distorted central vision (e.g., straight lines appearing wavy).

- A dark spot or blind area in the center of your vision.
- Difficulty reading, recognizing faces, or performing tasks requiring precise vision.
- Needing more light to read or perform activities.
- Colors appearing faded or muted.
- In advanced cases, AMD can cause significant central vision loss, severely impacting quality of life and making activities like reading or driving impossible.
What causes AMD?
AMD is primarily linked to the aging of the macula and genetic factors. However, certain risk factors can accelerate its onset or progression:
Non-modifiable risk factors:
- Age: Risk increases significantly after age 55–60.
- Family history: Having relatives with AMD increases your likelihood.
- Ethnicity: People of Caucasian descent and those with light-colored eyes have a slightly higher risk.
- Previous AMD: If one eye is affected, the risk is higher for the other eye.
Modifiable risk factors (ones you can control):
- Smoking: The most significant preventable risk factor, doubling or tripling the risk of AMD.
- High blood pressure, high cholesterol, obesity, and sedentary lifestyle: These conditions can worsen eye health.
- Poor diet: A lack of green leafy vegetables, oily fish, or nuts can increase the risk.
- Intense sun exposure: Unprotected UV exposure can damage the retina.
How is AMD diagnosed, and why is early diagnosis important?
Early diagnosis is critical to slowing the progression of AMD and preserving vision. Regular eye check-ups are recommended starting at age 40–45, or earlier if there’s a family history.
Diagnostic procedures
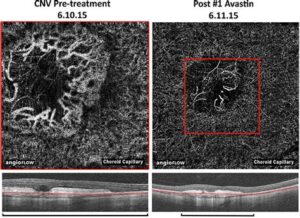
- OCT (Optical Coherence Tomography): Provides detailed images of the retina to detect macular changes.
- OCT-A (Angiography OCT): Assesses blood flow in the retina without injections.
- Dilated fundus exam: Allows the ophthalmologist to examine the retina in detail.
These procedures are quick, non-invasive, and essential for accurate diagnosis.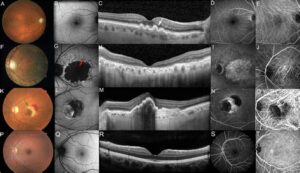
How to reduce the risk: Healthy lifestyle tips
Adopting healthy habits can help prevent or delay the progression of AMD:
- Quit smoking: Avoid tobacco, including secondhand smoke, as it’s the most significant risk factor.
- Follow a Mediterranean diet: Prioritize green leafy vegetables (spinach, kale), fruits, oily fish (sardines, salmon), legumes, and nuts. Limit ultra-processed foods and sugars.
- Exercise regularly: Maintain a healthy weight and good circulation.
- Protect your eyes from the sun: Wear sunglasses with high-quality UV filters.
- Manage other health conditions: Keep blood pressure, cholesterol, and diabetes under control with your doctor’s guidance.
- Get enough sleep: Adequate rest supports overall health, including eye health.
Treatments for AMD
Early-stage treatment:
- Antioxidant supplements (AREDS2 formula): Combinations of lutein, zeaxanthin, zinc, and copper may slow progression in some cases. Take them only under your ophthalmologist’s prescription and guidance.
Advanced-stage treatment (wet AMD):
- Anti-VEGF medications:
- Laser therapies:
- Photodynamic therapy or thermal laser may be used in specific cases when anti-VEGF injections are not effective or suitable.
- Treatment is individualized and determined by your specialist.
Final message
Early detection and regular follow-ups with your ophthalmologist are the best ways to protect your vision. Combine this with a healthy lifestyle and proper management of other health conditions. If you notice any changes in your vision, such as blurriness, distorted lines, or dark spots, consult your ophthalmologist immediately.
Acting promptly can make all the difference!
The retina is the inner layer that lines the back oft he eye. It mainly consists of nerve fibres and light receptors and its role is to capture the light which reaches the eye and send information about it to the visual part of the brain.
The macula is the central spot in the middle of the retina. It contains the highest density of light receptors and the lens system of the eye focuses images exactly on it. It is, therefore, responsible for the sharp vision and for the vision of colours.
What are the most common retinal diseases?
- Age related macula degeneration (dry and wet): macular degeneration is the leading cause of legal blindness among the elderly population.
- Epiretinal membranes.
- Macular hole.
- Posterior vitreous detachment and vitreous floaters.
- Retinal detachment.
- Diabetic retinopathy wit or without macular affection.
- Macular oedema.
- Retinal vessel occlusions (retinal “strokes”).
- Retinitis pigmentosa.
For detailed information, visit: http://www.evrs.eu/library-of-retinal-disease/
Because they can produce devastating and permanent visual impairment, leading to functional or total blindness.
Decades ago, there were almost no treatment options for macular degeneration and many other diseases of the retina. Nevertheless, with the development of modern diagnostic technology, as well as of modern microsurgery, lasers and medication (see below), cases that were untreatable just years ago, have become successfully treated nowadays. Still there are many issues left, but medical research shows promising developments for a near future.
- Optical Biomicroscopy
- Retinography
- OCT (Optical Coherence Tomography)
- Fluorescein angiography
- Ultrasound scan
- Electrophysiology: Evoked potentials / Electroretinography
Medication:
- Eye drops and tablets: Antiinflammatories, antibiotics
- Vitamins as nutritional supplements
- Tablets: Blood thinners, Corticosteroids
- Medication for intraocular (intraviteal) injection in cases of Macular degeneration:
- Macugen® (Pegabtanib)
- Avastin® (Bevacizumab) / Lucentis® (Ranimizumab): http://www.lucentis.com/information
- Eylea® (Aflibercept): http://www.eylea.co.uk/patients/wet-amd/index.php
- Corticosteroids used in cases of diabetic macular oedema:
- Triamcinolone
- Ozurdex® (Dexamethasone): http://www.ozurdex.com
Laser:
- Argonlaser
- Photodynamic Therapy
Surgery:
- Surgery of retinal detachment
- Vitrectomy: http://www.willseye.org/health-library/vitrectomy
- Macula Peeling
Magnifying and low-vision optical instruments:
A wide variety of rehabilitation options are available to help patients with low vision live and work more effectively, efficiently, and safely. Most people can be helped with one or more low vision treatment options.
The more commonly prescribed devices are:
- Spectacle-mounted
- Hand-held or spectacle-mounted telescopes
- Hand-held and stand magnifiers
- Video magnification
Several systems can be tried out in our office, before they might be prescribed.